Prof Cheng Teng Ip, assistant professor at The Centre for Cognitive and Brain Science of the University of Macau (UM), has conducted significant research on EEG Vigilance as a biomarker for predicting treatment responses to antidepressants. This research, which explores the association between EEG Vigilance Regulation and Ketamine treatment, has been accepted for publication in the journal Translational Psychiatry.
Depression is a debilitating mental disorder that can be resistant to conventional treatments such as serotonin and noradrenaline reuptake inhibitors (SNRIs). While witnessed promising interventions like ketamine show efficacy in therapy-resistant depressive disorder cases, due to its rapid onset of action and effectiveness in patients who have not responded adequately to conventional antidepressant agents. Despite its benefits, around 50% of patients do not respond to a single infusion, necessitating a more targeted approach. A more stratified psychiatry is needed to pinpoint patients who are most likely to benefit from a ketamine intervention.
Electroencephalogram (EEG) offers a non-invasive and cost-effective method for directly measuring brain function when compared to other sophisticated device-based biomarkers. The EEG vigilance, after the term was coined a century ago by British neurologist Sir Henry Head, is widely used in the electrophysiological framework for affective disorders. The EEG Vigilance Regulation Patterns, an algorithm developed, validated, and replicated, serves to categorize 1s EEG epoch into distinct vigilance stages, including stages 0, A1, A2/3, B1, B2/3, and sleep stage C. Most individuals naturally undergo transitions between these different vigilance stages as part of their physiologic vigilance regulation. Notably, previous research has unveiled a shift of EEG spectra towards slow and fast oscillations following ketamine administration. In alignment with clinical observations, previous studies indicate that responders to fluoxetine exhibit higher pretreatment occipital absolute alpha power compared to non-responders and healthy controls. Furthermore, lower relative delta and theta powers have been associated with improved treatment responses to paroxetine. Recent replication in a substantial, independent cohort reinforces the findings that the EEG vigilance algorithm exhibits commendable diagnostic and predictive capabilities in major depressive disorder (MDD). Specifically, a swift transition to lower vigilance stages has emerged as a reliable predictor of a favorable response to SSRI treatment. Moreover, ongoing research has identified a correlation between baseline EEG activity and the response to ketamine in individuals with MDD.
The study aimed to identify predictors of response to a single intravenous dose of ketamine as a treatment for depression in patients with MDD. The dataset comes from a double-blind, placebo-controlled, randomized, crossover study where patients aged 18–65 years suffering from MDD, received a placebo infusion followed by a ketamine infusion after 7 days and were assessed by the Montgomery–Åsberg Depression Rating Scale (MADRS). Then, the research team quantified and compared the EEG vigilance assessments in two distinct cohorts (original dataset n=24 and testing dataset n=24).
Key findings indicated a distinguishable decrease in EEG wakefulness after the second infusion, especially in stage B1, suggesting a ketamine-specific effect. Moreover, dose-dependency was evident, correlating an increase in stage B1 with higher serum Ketamin concentration. Group effects emerged in median vigilance, stages A1 and B2/3. Specifically, responders demonstrated a more rapid decline in median vigilance and had a heightened tendency for drowsiness compared to non-responders. Subsequent investigations unveiled that, at pre-infusion, responders showed a significantly higher percentage of stage A1 compared to non-responders. This pre-infusion difference for stage A1 between responders and non-responders was found in both ketamine and placebo interventions, suggesting a consistent trait aspect in vigilance regulation for response or non-response. After Utilizing percentages of A1 stages as a predictive marker for treatment response, the result revealed if the percentage of A1 stages is above 43% within the first 10 minutes of EEG recording, the patient in the testing set had 4.2 times higher odds of being responders.
Prof. IP is the first author of this research, and Prof. Sebastian Olbrich from the University of Zurich is the corresponding author. Prof. Martin Brunovsky Provided the data included in the study by the Ministry of Health of the Czech Republic (NV18-04-00260 and NV17-32478A), and by the Charles University project (PROGRES Q35 and LO1611). The research is supported by the University of Macau (File no: SRG2023-00040-ICI), Augustinusfonden (19-0219), and the Lundbeck Foundation (BrainDrugs: R279-2018-1145). The full version of the article can be viewed at: https://www.nature.com/articles/s41398-024-02761-x.pdf
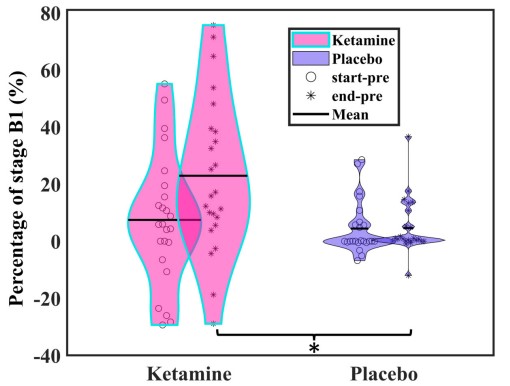
Ketamine increases the amount of low vigilance stage B1
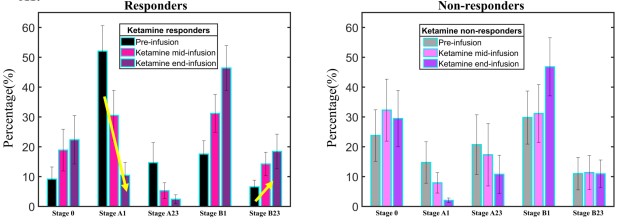
Ketamine effects on different vigilance stages
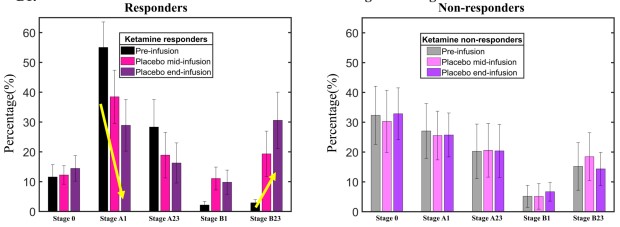
Placebo effects on different vigilance stages
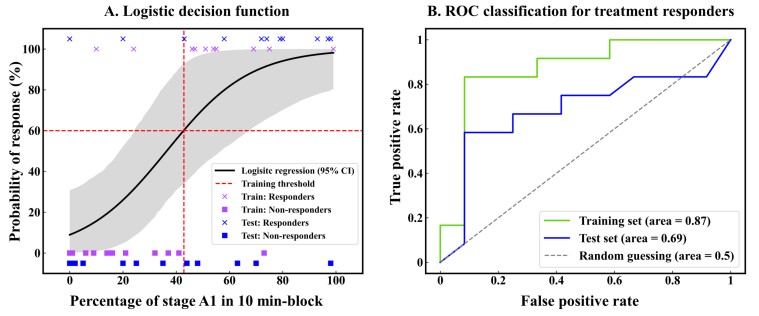
Vigilance tage A1 serves as a biomarker for treatment responses