Led by Assistant Professor Cheng Teng, Ip from the Centre for Cognitive and Brain Sciences at the University of Macau (UM), an international research collaboration with Denmark has made a significant discovery. The study revealed that Electroencephalography (EEG) abnormalities do not correlate with the efficacy of antidepressant treatments. Therefore, it is advised not to include EEG abnormalities in the treatment-choice decision tree for antidepressant strategies. The research results have been accepted by the prestigious international journal, European Neuropsychopharmacology.
Depression is a very common and complex mental illness, and despite several antidepressant options available, patients often struggle to find effective treatment. First-line antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), do not promote relief in most patients with major depressive disorder (MDD). Therefore, there is a need to identify an intuitive predictive marker of treatment response to guide the selection of treatment strategies and improve the accuracy of care for patients with poor responses to multiple antidepressants.
EEG has been considered a potential clinical tool for predicting treatment outcomes in depression. However, its effectiveness is currently limited due to the lack of out-of-sample validation and replication of existing studies. Prior research has indicated that certain abnormal EEG activities, like isolated epileptiform discharges (IEDs) and EEG slowing, might serve as biomarkers for non-response to specific antidepressants. This underscores the complexity of using EEG in clinical settings and the need for further rigorous studies to validate its predictive capabilities in treating depression.
The research team is focused on examining whether EEG abnormalities correlate with a poor response to SSRI treatment in patients with severe depression, specifically during a 12-week open-label treatment with escitalopram. In addition, the team is exploring the potential relationship between EEG abnormalities and differences in emotional, anxiety, or cognitive functions among these patients. The study reports findings of NeuroPharm study, a longitudinal, open-label multimodal neuroimaging clinical trial investigating potential biomarkers in the antidepressant treatment of MDD conducted by Prof Ip. In this study, a total of 91 patients aged 18-65 years, diagnosed with moderate to severe depression episodes lasting less than two years, were evaluated and included. The dosage, ranging from 10-20 mg daily, was individually adjusted based on each patient’s response to the treatment and any side effects experienced. The severity of depression was evaluated using the Hamilton Depression Rating Scale (HAMD17) before treatment, at week 4, week 8, and week 12 of treatment period.
The study’s findings indicate no significant difference in the severity of depression among patients, regardless of the presence or absence of EEG abnormalities. This suggests that abnormal EEG patterns may not serve as a reliable, generalizable, and operable biomarker for predicting outcomes of SSRI treatment. Consequently, their use in routine clinical practice is not recommended without further validation. Additionally, the study uncovers a correlation between EEG abnormalities in the pretreatment depressive state and issues related to emotional disorders and verbal memory deficits. These insights pave the way for more focused research on EEG abnormalities. Such research could play a crucial role in optimizing treatment strategies for patients with cognitive and emotional deficiencies, ultimately improving treatment outcomes.
Prof. Ip is the last and corresponding author of this research, collaborating closely with Kristian Reveles, MD, from the University of Copenhagen. The research is supported by the University of Macau (SRG2023–00040-ICI), Augustinus Fonden (19–0219), the Research Fund of the Mental Health Services – Capital Region of Denmark, and the Lundbeck Foundation alliance BrainDrugs (R279–2018–1145). The full version of the article can be viewed at: https://doi.org/10.1016/j.euroneuro.2023.11.004
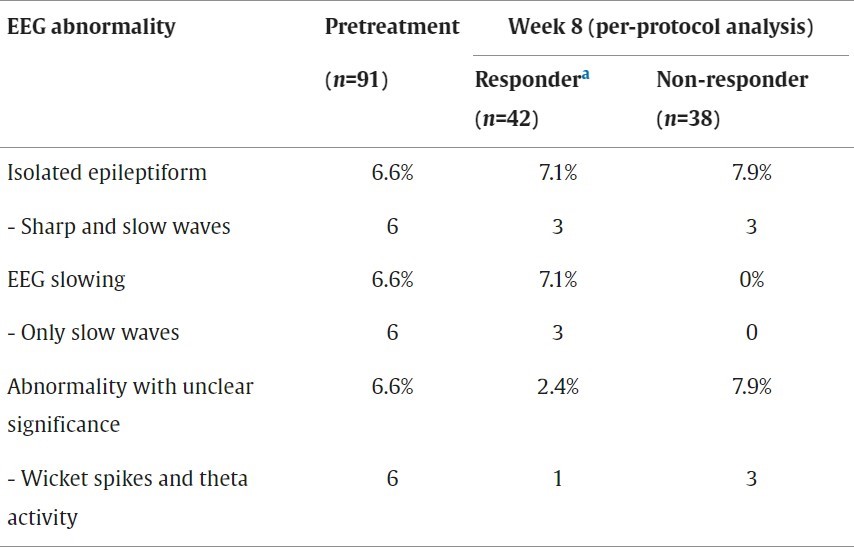
Frequency of EEG abnormalities
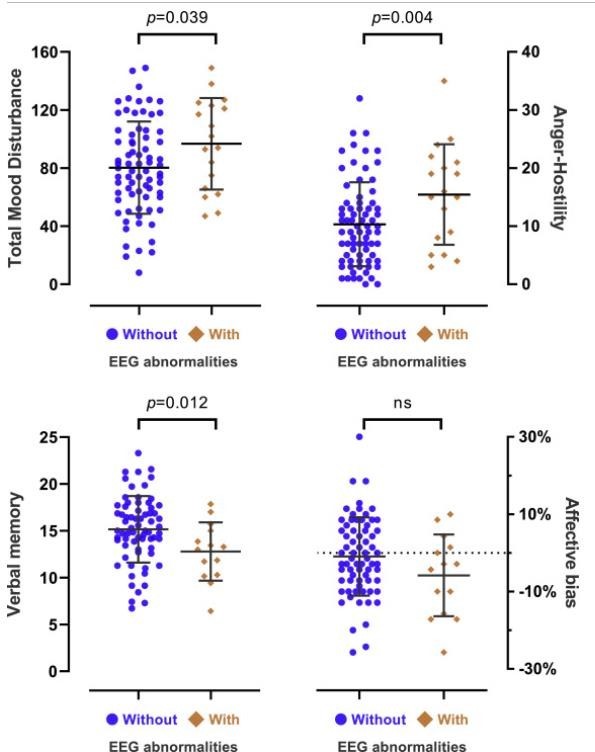
Pretreatment mood and cognitive differences